Introduction
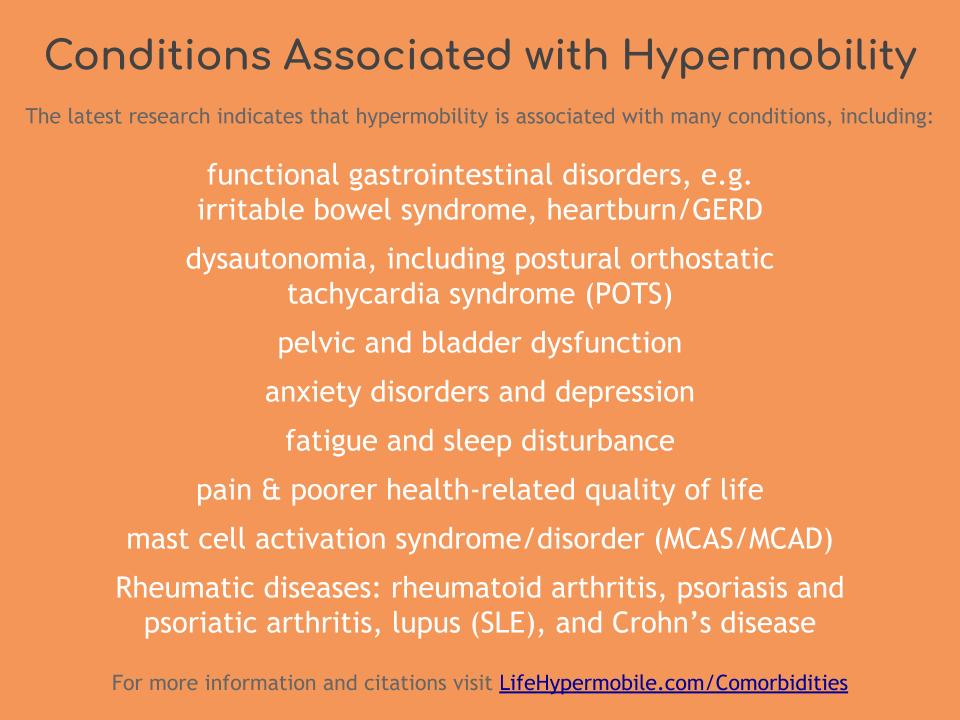
It is well established in the medical literature that hypermobility is associated with other conditions. According to the latest research,
“The literature is full of case-control studies showing a significant association between GJH [generalized joint hypermobility] (usually assessed by the Beighton score) and specific extra-articular disorders. To date, the strongest associations are with anxiety disorders, orthostatic tachycardia, a variety of functional gastrointestinal disorders, and pelvic and bladder dysfunction. These associations are often real (i.e. easily confirmed by clinical practice) and clinically relevant as these additional manifestations may be commonly encountered in conditions with JH [joint hypermobility], in particular hEDS, and might impact seriously on the quality of life and management of affected individuals.”*
“Many other features are described in hEDS but most are not sufficiently specific nor sensitive at the moment to be included in formal diagnostic criteria… These include but are not limited to: sleep disturbance, fatigue, postural orthostatic tachycardia, functional gastrointestinal disorders, dysautonomia, anxiety, and depression. These other systemic manifestations may be more debilitating than the joint symptoms, often impair functionality and quality of life, and should always be determined during clinical encounters. While they are not part of the diagnostic criteria, the presence of such systemic manifestations may prompt consideration of hEDS in the differential diagnosis.”**
“hEDS is … multisystemic with primary musculoskeletal manifestations but various other comorbidities exist such as pain, fatigue, orthostasis, sleep disturbance, anxiety, and a poorer health-related quality of life.”***
Unfortunately, it’s too early to know WHY these conditions are so often found together. There isn’t enough evidence to truly determine if there is an underlying causal relationship, or whether there is simply a correlation.
Therefore, the latest researchers have concluded that,
“It is too premature to consider such manifestations primary (i.e. pleiotropic) clinical expressions of the underlying etiological factor (i.e. genetic mutation). Therefore, these complications, when encountered in patients belonging to one of the above mentioned categories of JH [see About Hypermobility Spectrum Disorders], should be defined as JH-related co-morbidities. The concurrence of JH and one or more of its co-morbidities does not exclude an accurate differential diagnosis for the other causes underlying such co-morbidities.”*
In Detail
Gastrointestinal Comorbidities
Pain and Hypermobility
Mast Cell Activation Syndrome (MCAS)
Rheumatic Diseases
Autonomic Dysfunction/Dysautonomia
Sources
*Castori M, Tinkle B, Levy H, Grahame R, Malfait F, Hakim A. 2017. A framework for the classification of joint hypermobility and related conditions. Am J Med Genet Part C Semin Med Genet 175C:148–157.
**Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, Bloom L, Bowen JM, Brady AF, Burrows NP, Castori M, Cohen H, Colombi M, Demirdas S, De Backer J, De Paepe A, Fournel-Gigleux S, Frank M, Ghali N, Giunta C, Grahame R, Hakim A, Jeunemaitre X, Johnson D, Juul-Kristensen B, Kapferer-Seebacher I, Kazkaz H, Kosho T, Lavallee ME, Levy H, Mendoza-Londono R, Pepin M, Pope FM, Reinstein E, Robert L, Rohrbach M, Sanders L, Sobey GJ, Van Damme T, Vandersteen A, van Mourik C, Voermans N, Wheeldon N, Zschocke J, Tinkle B. 2017. The 2017 international classification of the Ehlers–Danlos syndromes. Am J Med Genet Part C Semin Med Genet 175C:8–26.
***Tinkle B, Castori M, Berglund B, Cohen H, Grahame R, Kazkaz H, Levy H. 2017. Hypermobile Ehlers–Danlos syndrome (a.k.a. Ehlers–Danlos syndrome Type III and Ehlers–Danlos syndrome hypermobility type): Clinical description and natural history. Am J Med Genet Part C Semin Med Genet 175C:48–69.